#FEMSmicroBlog: How bacteria mess with your DNA: Lessons from Staphylococcus aureus and other pathogens
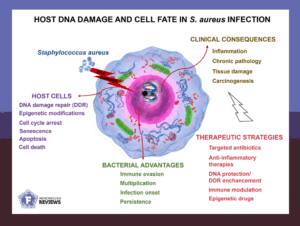
By causing infections, some bacterial pathogens alter the integrity of human cells more profoundly, influencing long-term health. For example, several bacteria harm the DNA of the cells they infect. The review “Host DNA damage and cellular fate in bacterial infections, with a focus on Staphylococcus aureus” in FEMS Microbiology Reviews outlines how diverse pathogens induce a damage that trigger complex DNA repair mechanisms. In this #FEMSmicroBlog, Nadia Nadeja Berkova explains how Staphylococcus aureus determines the balance between bacterial clearance and persistence. #FascinatingMicrobes
When bacteria break the rules: infection and genome modifications
When a human cell detects DNA damage, it triggers the cell’s DNA Damage Response. This coordinated network of sensors, signalling pathways, and repair mechanisms is tasked to maintain genomic integrity.
Some pathogenic bacteria, however, are capable of exploiting these responses, and creating persistent infections and long-term changes in cellular behaviour. For example:
- Escherichia coli produces colibactin, a toxin that induces double-strand DNA breaks
- Campylobacter releases Cytolethal Distending Toxin, which disrupts DNA and halts cell division
- Helicobacter pylori triggers oxidative stress, causing DNA lesions and abnormal DNA methylation, a form of epigenetic reprogramming that can persist after infection
- Fusobacterium nucleatum and Actinomyces odontolyticus release vesicles and nucleases that induce DNA damage and modify histones
These bacterial effectors both damage the DNA and interfere with components of the DNA Damage Response itself. For example, they may modulate repair enzyme activity, alter signaling pathways, or reshape the chromatin. The resulting lesions and epigenetic changes disrupt cell function, promote inflammation, and lead to long-lasting tissue alterations.
DNA under siege: What Staphylococcus aureus reveals about persistent infections
Staphylococcus aureus is a major cause of chronic and life-threatening infections worldwide. Antibiotic-resistant strains, including MRSA and multidrug-resistant variants, survive aggressive therapies, prolonging illness and increasing complications.
Beyond antibiotic resistance, Staphylococcus aureus is also a master of manipulating host cells. This is discussed in the review “Host DNA damage and cellular fate in bacterial infections, with a focus on Staphylococcus aureus” published in FEMS Microbiology Reviews.
For host cell manipulation, Staphylococcus aureus produces specialised effector molecules, with some of them entering the nucleus to directly modify histones and chromatin. Others, such as cyclomodulins, act in the cytosol, where they disrupt cell cycle regulators, ultimately affecting nuclear processes. These alterations reduce immune cell responsiveness, allowing bacteria to persist and contributing to recurrent infections, slow-healing wounds, and prolonged inflammation.
As some of these effectors disrupt metabolism and generate oxidative stress, they damage the DNA and activate the DNA Damage Response. An additional set of effectors directly interferes with components of the DNA Damage Response, which can promote tissue remodelling.
Together, these strategies impair immune responses and create an environment favourable for bacterial persistence, often leading to scarring and, in some cases, an increased cancer risk. The combination of DNA damage, immune evasion, epigenetic reprogramming, and antibiotic resistance makes Staphylococcus aureus a highly virulent pathogen.
Fighting back: rethinking therapy against DNA-damaging bacteria
Since Staphylococcus aureus is both an infectious and DNA-damaging agent, we need to reshape therapeutic strategies to fight it. Antibiotics may not be enough.
One way could be to boost the trained immunity. This involves priming innate immune cells with microbial or metabolic signals that trigger metabolic and epigenetic reprogramming, preparing them for stronger responses to infections.
Since trained immunity depends on epigenetic marks, protecting DNA and correcting harmful epigenetic changes can help maintain this primed state. Together, these mechanisms may limit tissue damage and improve recovery, even after infections with resistant strains.
Staphylococcus aureus, as both a toxin-producing and genotoxic pathogen, causes lasting health effects. Combining antibiotics with host-directed therapies may better prevent chronic infections and tissue damage, offering more effective treatments against MRSA and other resistant strains.
- Read the article “Host DNA damage and cellular fate in bacterial infections, with a focus on Staphylococcus aureus” by Berkova et al. in FEMS Microbiology Reviews (2025).

Nadia Nadejda Berkova is a Research Director at INRAE, France. She has lead multiple research programs, including work at a CNRS genetics laboratory, France, and as an Associate Professor in the Faculty of Medicine at Laval University in Québec, Canada. Her work revealed how Staphylococcus aureus reprograms host cells—disrupting immune and transcriptional responses, altering cell-cycle progression, and inducing DNA damage through defined molecular mechanisms. Recently, she was exploring probiotic-induced trained immunity as a promising strategy to combat S. aureus infections.
About this blog section
The section #FascinatingMicrobes for the #FEMSmicroBlog explains the science behind a paper and highlights the significance and broader context of a recent finding. One of the main goals is to share the fascinating spectrum of microbes across all fields of microbiology.
| Do you want to be a guest contributor? |
| The #FEMSmicroBlog welcomes external bloggers, writers and SciComm enthusiasts. Get in touch if you want to share your idea for a blog entry with us! |
